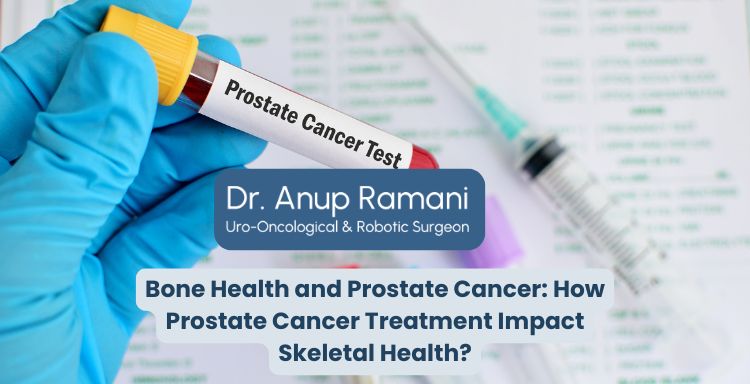
Bone Health and Prostate Cancer: How Prostate Cancer Treatment Impact Skeletal Health?
By Dr. Anup Ramani
Listening Article
About Author

Uro-Oncological & Robotic Surgeon
Dr. Anup Ramani is a robotic uro-oncological surgeon and an internationally recognized expert in robotic surgery for prostate, kidney and urinary bladder cancers. With more than two decades of robotic experience and 2,000+ robotic procedures, he brings unmatched precision and outcomes to complex uro-oncology cases. He is widely published in his field and is known for a personal, transparent approach-often spending over an hour in initial consultations to educate patients on its disease, surgery and recovery. His expertise spans prostate cancer treatment, kidney and bladder cancer surgery, adrenal gland surgery, kidney stone treatment, penile cancer surgery and enlarged prostate management. Dr. Ramani advocates the advantages of robotic surgery-magnified 3D vision, tremor-filtered precision, minimal scarring, lower blood loss and faster recovery-helping patients return to life sooner.
Table of Contents