Dr Anup Ramani @ Copyright 2024
By Dr. Anup Ramani
1. Introduction to Prostate Cancer
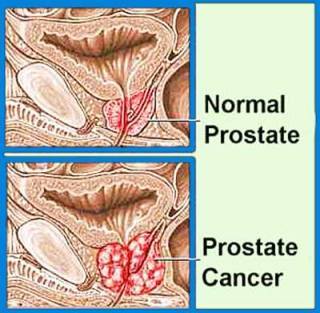
What is Prostate Cancer?
Prostate cancer is a type of cancer that develops in the prostate gland, which is part of the male reproductive system. It can vary from slow-growing to aggressive forms.
Impact on men's health worldwide
Prostate cancer is one of the most common cancers among men globally, with significant variations in incidence based on age, genetics, and lifestyle factors.
Importance of Early Detection
Early detection through screening tests like PSA (Prostate-Specific Antigen) tests and Digital Rectal Exams (DREs) is crucial for timely treatment.
Benefits of early diagnosis
- Early diagnosis increases the chances of successful treatment and improves survival rates.
- Allows for less invasive treatment options and better preservation of quality of life.
2. Understanding Prostate Cancer
Risk Factors for Prostate Cancer
- Age, family history, race
- Prostate cancer risk increases with age, especially after 50. Men with a family history of prostate cancer or certain genetic mutations are at higher risk.
- African-American men have a higher incidence and mortality rate compared to other racial groups.
- Lifestyle factors (diet, exercise)
- High-fat diets, obesity, lack of exercise, and smoking may increase the risk of developing prostate cancer.
Types and Stages of Prostate Cancer
Localized vs. advanced prostate cancer
- Localized cancer is confined to the prostate gland, while advanced cancer has spread beyond the prostate to other parts of the body.
Gleason score and tumor grading
- The Gleason score assesses the aggressiveness of prostate cancer cells based on their pattern of growth. Higher scores indicate more aggressive cancer.
3. Diagnosis of Prostate Cancer
Screening Methods (PSA Test, Digital Rectal Exam)
How PSA levels are measured
- PSA is a protein produced by the prostate gland. Elevated PSA levels can indicate prostate cancer or other prostate conditions.
- Regular PSA tests help monitor changes in PSA levels over time.
Procedure and frequency of DRE
- DRE involves a doctor examining the prostate gland through the rectum to feel for abnormalities such as lumps or hard areas.
- DRE is often performed alongside PSA testing for comprehensive screening.
Biopsy Procedure and Results
Indications for prostate biopsy
- A biopsy is recommended if PSA levels are elevated or if DRE detects suspicious changes in the prostate gland.
- During a biopsy, small tissue samples are taken from the prostate gland and examined under a microscope for cancer cells.
Interpreting biopsy results and Gleason score
- Biopsy results determine the presence of cancer, its stage, and the Gleason score, which guides treatment decisions.
4. Treatment Options Overview
Active Surveillance
Criteria for active surveillance
- Active surveillance involves closely monitoring low-risk prostate cancer without immediate treatment, intervening only if the cancer progresses.
- Regular PSA tests, DREs, and occasional biopsies are performed to monitor cancer progression.
Monitoring prostate cancer progression
- Periodic imaging tests (MRI, ultrasound) and biomarker tests may also be used to assess changes in cancer activity over time.
Surgery (Prostatectomy)
Overview of surgical removal of the prostate
- Prostatectomy is the surgical removal of the prostate gland and possibly nearby tissues.
- It is considered for localized prostate cancer that has not spread beyond the prostate gland.
Comparison of open, laparoscopic, and robotic techniques
- Open surgery involves a single large incision, laparoscopic surgery uses small incisions and a camera for visualization, and robotic surgery offers enhanced precision and quicker recovery.
Radiation Therapy
Types of radiation treatment (external beam, brachytherapy)
- External beam radiation delivers targeted radiation to the prostate from outside the body.
- Brachytherapy involves implanting radioactive seeds directly into the prostate gland to deliver radiation internally.
How radiation therapy targets prostate cancer cells
- Radiation damages cancer cells’ DNA, preventing them from dividing and growing.
- Treatment sessions are typically spread out over several weeks to allow healthy cells to recover between sessions.
5. Surgical Treatment: Prostatectomy
Types of Prostatectomy (Open, Laparoscopic, Robotic)
Detailed explanation of each technique
- Open prostatectomy provides direct access to the prostate but involves a longer recovery period.
- Laparoscopic prostatectomy uses small incisions and specialized tools for surgery, reducing recovery time compared to open surgery.
- Robotic-assisted prostatectomy offers precise control and minimal invasiveness, leading to faster recovery and fewer complications.
Benefits and Risks
Benefits of surgical removal
- Complete removal of cancerous tissue from the prostate gland.
- Potential for cure, especially for early-stage prostate cancer.
Potential risks and complications
- Erectile dysfunction and urinary incontinence are common but often improve over time.
- Infection, bleeding, and damage to surrounding tissues are possible complications.
6. Preparing for Prostate Surgery
Preoperative Consultation
Meeting with urologist and anesthesiologist
- Discussing surgical options, risks, and expected outcomes.
- Anesthesiologist evaluates medical history to determine anesthesia type and risks.
Medical tests and evaluations before surgery
- Blood tests, electrocardiogram (ECG), and imaging tests may be conducted to assess overall health and fitness for surgery.
- Medication adjustments may be necessary to optimize surgical outcomes and minimize risks.
Steps to Prepare Mentally and Physically
Psychological readiness for surgery
- Addressing concerns, fears, and expectations about surgery and recovery.
- Engaging in relaxation techniques, counseling, or support groups for emotional preparation.
Physical preparation and lifestyle adjustments
- Following dietary guidelines, quitting smoking, and increasing physical activity to improve overall health before surgery.
- Arranging transportation and support for postoperative care and recovery at home.
7. Procedure Details: What to Expect
Operating Room Setup
Sterile environment and surgical team roles
- Ensuring cleanliness and infection control measures in the operating room.
- Roles of surgeons, nurses, and technicians during surgery to ensure patient safety and procedural efficiency.
Equipment used during prostatectomy
- Surgical instruments, robotic systems (if applicable), anesthesia equipment, and monitoring devices used during surgery.
- Advanced imaging tools like MRI or ultrasound may assist in precise surgical navigation.
8. During Surgery: Surgical Techniques
Removal of Prostate Tissue
Step-by-step process of prostate removal
- Separating the prostate gland from surrounding tissues while preserving nerves and blood vessels critical for urinary and sexual function.
- Ensuring complete removal of cancerous tissue while minimizing damage to healthy tissues.
Preservation of surrounding structures (nerves, bladder)
- Techniques such as nerve-sparing surgery aim to preserve erectile function by avoiding damage to nerves responsible for sexual arousal.
- Maintaining bladder function by carefully reconnecting the bladder to the urethra after prostate removal.

9. Recovery Phase: Postoperative Care
Robotic Hospital Stay and Monitoring
Duration of hospitalization
- Typically 1-3 days depending on the surgical approach and individual recovery progress.
- Monitoring vital signs, pain levels, and initial urinary function to detect early complications.
Managing Pain and Potential Complications
- Pain management strategies post-surgery
- Administering pain medications through intravenous (IV) or oral routes to control discomfort.
- Encouraging early mobility and breathing exercises to prevent complications like pneumonia or blood clots.
- Common complications and how they are treated
- Addressing urinary catheter-related discomfort, constipation, or incisional pain through medication and supportive care.
- Monitoring for signs of infection or bleeding and taking prompt action to prevent complications.
10. Rehabilitation and Physiotherapy
Regaining Bladder Control (Kegel Exercises)
Importance of pelvic floor exercises
- Strengthening pelvic floor muscles to regain urinary control and prevent urinary leakage (incontinence).
- Performing Kegel exercises regularly under the guidance of healthcare providers to improve muscle tone and control.
Timeline for regaining urinary continence
- Gradual improvement in bladder control over weeks to months post-surgery, with some patients achieving full continence sooner than others.
Sexual Function Rehabilitation
Impact of surgery on sexual function
- Temporary or permanent erectile dysfunction (impotence) due to nerve damage or trauma during surgery.
- Managing expectations and exploring treatment options like medications or penile implants to restore sexual function.
Strategies for restoring erectile function post-surgery
- Engaging in sexual counseling, exploring intimacy techniques, and using supportive aids to enhance sexual satisfaction and intimacy.
- Patience and open communication with partners to navigate changes in sexual health and intimacy.
11. Long-Term Effects and Lifestyle Changes
Continence Issues
Strategies for managing urinary incontinence long-term
- Using absorbent pads or adult diapers temporarily to manage leakage.
- Practicing timed voiding, limiting caffeine intake, and maintaining a healthy weight to support bladder control.
When to seek help from a specialist
- Consulting urologists or continence nurses for persistent incontinence issues or worsening symptoms despite conservative management.
- Exploring advanced treatments like surgery or injectable therapies for severe urinary incontinence.
Psychological Impact and Support Resources
Coping with emotional challenges post-surgery
- Addressing anxiety, depression, or body image concerns through individual counseling or support groups.
- Utilizing online forums, peer support networks, or community organizations to connect with other prostate cancer survivors.
Support groups and counseling services for patients and families
- Accessing educational resources, workshops, or retreats tailored to prostate cancer patients and their loved ones.
- Providing emotional support and practical guidance on navigating treatment decisions, survivorship, and quality of life issues.
12. Radiation Therapy as an Alternative
Types of Radiation (External Beam, Brachytherapy)
How external beam radiation targets prostate cancer cells
- Delivering high-energy X-rays to the prostate gland from outside the body to destroy cancer cells.
- Daily treatment sessions over several weeks to ensure targeted delivery of radiation while minimizing damage to nearby healthy tissues.
Implantation of radioactive seeds in brachytherapy
- Inserting small radioactive pellets (seeds) directly into the prostate gland to emit radiation and kill cancer cells over time.
- Monitoring radiation exposure and ensuring patient safety during and after seed implantation procedures.
How Radiation Works Against Cancer Cells
Mechanism of action in damaging cancer DNA
- Interfering with cancer cell division and growth by damaging their genetic material (DNA).
- Triggering apoptosis (cell death) in cancer cells while sparing surrounding healthy tissues to reduce treatment-related side effects.
Side effects and management during radiation therapy
- Addressing temporary side effects like fatigue, skin irritation, or gastrointestinal symptoms through supportive care measures.
- Monitoring long-term effects such as urinary or bowel changes and providing ongoing medical management or symptom relief.
13. Combination Therapies and Clinical Trials
Hormone Therapy
Role of hormone therapy in prostate cancer treatment
- Suppressing testosterone levels to slow prostate cancer growth and shrink tumors.
- Administering hormone therapy alone or in combination with other treatments like surgery or radiation therapy to improve outcomes.
Side effects and benefits of hormone therapy
- Managing hormonal changes, hot flashes, and sexual dysfunction through medications or lifestyle modifications.
- Monitoring bone health and cardiovascular risks associated with long-term hormone therapy use in prostate cancer patients.
Immunotherapy and Targeted Therapy
Emerging treatments targeting specific prostate cancer markers
- Harnessing the immune system to recognize and destroy cancer cells with checkpoint inhibitors or vaccines.
- Investigating targeted therapies that block specific pathways or genetic mutations driving prostate cancer growth in clinical trials.
Clinical trials investigating new treatment combinations
- Participating in research studies to evaluate novel therapies, combination treatments, or personalized medicine approaches for advanced prostate cancer.
- Collaborating with healthcare providers and research teams to access cutting-edge treatments and contribute to future advancements in prostate cancer care.

14. Managing Recurrence: What to Know
Signs of Recurrence
Monitoring PSA levels for recurrence
- Tracking changes in PSA blood levels as an indicator of cancer recurrence or disease progression.
- Establishing personalized monitoring schedules and diagnostic tests to detect early signs of recurrent prostate cancer.
Symptoms indicating cancer recurrence
- Recognizing symptoms such as bone pain, urinary problems, or unexplained weight loss that may indicate recurrent prostate cancer.
- Consulting healthcare providers promptly to initiate diagnostic evaluations and treatment adjustments as needed.
Treatment Options for Recurrent Prostate Cancer
Salvage therapies after recurrence
- Exploring secondary treatments like salvage prostatectomy, radiation therapy, or hormone therapy to manage recurrent prostate cancer.
- Discussing potential benefits, risks, and outcomes with specialists to tailor treatment plans based on individual health status and cancer characteristics.
Palliative care and symptom management
- Emphasizing quality of life by addressing pain, discomfort, or psychological distress associated with advanced prostate cancer.
- Collaborating with palliative care teams to provide comprehensive support, symptom relief, and end-of-life care options for patients and their families.
15. Integrative Approaches to Support Treatment
Nutrition and Diet Recommendations
Foods that support prostate health
- Incorporating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to promote overall well-being and immune function.
- Choosing heart-healthy fats, limiting red meat and processed foods, and staying hydrated to support prostate health and reduce cancer risk.
Nutritional strategies during and after treatment
- Adjusting dietary habits to manage treatment-related side effects like nausea, fatigue, or changes in appetite.
- Consulting registered dietitians or nutrition specialists for personalized meal plans, supplements, or dietary guidelines to optimize recovery and maintain nutritional balance.
Role of Exercise and Stress Management
Benefits of physical activity for recovery
- Engaging in regular exercise to improve muscle strength, cardiovascular health, and overall physical function during prostate cancer treatment.
- Incorporating aerobic activities, strength training, and flexibility exercises to enhance energy levels, reduce stress, and promote mental well-being.
Stress reduction techniques for overall well-being
- Practicing mindfulness, relaxation techniques, or yoga to alleviate stress, anxiety, and emotional strain associated with prostate cancer diagnosis and treatment.
- Participating in support groups, counseling sessions, or stress management programs to cultivate resilience, coping skills, and a positive outlook on recovery.
16. Patient Perspectives: Real Stories
Testimonials and Personal Experiences
- Sharing patient stories, journeys, and insights into navigating prostate cancer diagnosis, treatment decisions, and survivorship.
- Providing firsthand perspectives on challenges, triumphs, and lessons learned from living with prostate cancer and supporting loved ones through the journey.
17. Frequently Asked Questions (FAQs)
How is prostate cancer diagnosed?
Explaining screening tests, diagnostic procedures, and the role of healthcare providers in diagnosing prostate cancer early.
What are the risks of prostate surgery?
Discussing potential complications, recovery expectations, and surgical risks associated with different prostatectomy techniques.
Can prostate cancer be prevented?
Addressing lifestyle modifications, screening recommendations, and preventive strategies to reduce prostate cancer risk and promote overall health.
How long does it take to recover from prostate surgery?
Outlining recovery timelines, postoperative care tips, and factors influencing individual recovery after prostate cancer surgery.
What are the alternatives to surgery for prostate cancer?
Exploring non-surgical treatment options such as radiation therapy, hormone therapy, active surveillance, or participation in clinical trials for prostate cancer management.
18. Research and Advancements in Prostate Cancer Treatment
Latest Innovations in Surgical Techniques
- Highlighting technological advancements, robotic-assisted surgery, and minimally invasive approaches for precision and improved outcomes in prostatectomy.
Emerging Therapies and Clinical Trials
- Discussing innovative treatments, targeted therapies, immunotherapy advancements, and personalized medicine strategies shaping the future of prostate cancer care.
Role of genomic testing in personalized treatment plans
- Utilizing genetic testing, biomarker analysis, and genomic profiling to tailor treatment strategies, predict treatment response, and optimize therapeutic outcomes in prostate cancer patients.

19. Support Systems for Patients and Families
Counseling and Support Groups
- Recognizing the emotional impact of prostate cancer on patients and families and providing access to professional counseling, peer support networks, and educational resources.
Importance of emotional support during treatment
- Offering compassionate care, practical guidance, and holistic support services to address psychosocial needs, anxiety, and adjustment to life changes following prostate cancer diagnosis and treatment.
Resources for finding local support groups
- Connecting patients, caregivers, and loved ones with community-based organizations, online forums, and national advocacy groups offering information, support, and encouragement throughout the prostate cancer journey.
Financial Assistance and Insurance Coverage
- Navigating healthcare costs, insurance coverage, financial resources, and patient assistance programs to alleviate financial burdens and ensure equitable access to prostate cancer treatment and supportive care services.
Comprehensive support for patients and families
- Collaborating with multidisciplinary healthcare teams, social workers, and patient navigators to coordinate care, address practical needs, and empower individuals affected by prostate cancer to make informed decisions and enhance quality of life.
20. Conclusion: Hope and Future Outlook
Importance of Early Detection and Treatment
- Emphasizing the pivotal role of early diagnosis, proactive screening, and timely intervention in improving prostate cancer outcomes, reducing mortality rates, and promoting long-term survivorship.
Impact of early diagnosis on treatment outcomes
- Celebrating advancements in prostate cancer research, treatment modalities, and supportive care initiatives that contribute to enhanced quality of life, survivorship, and hope for the future.
Public health initiatives promoting prostate cancer awareness
- Advocating for public awareness campaigns, health education efforts, and community outreach programs to empower individuals, raise awareness, and foster proactive engagement in prostate cancer prevention, screening, and comprehensive care.
About Author

Uro-Oncological & Robotic Surgeon
Dr. Anup Ramani is a robotic uro-oncological surgeon and an internationally recognized expert in robotic surgery for prostate, kidney and urinary bladder cancers. With more than two decades of robotic experience and 2,000+ robotic procedures, he brings unmatched precision and outcomes to complex uro-oncology cases. He is widely published in his field and is known for a personal, transparent approach-often spending over an hour in initial consultations to educate patients on its disease, surgery and recovery. His expertise spans prostate cancer treatment, kidney and bladder cancer surgery, adrenal gland surgery, kidney stone treatment, penile cancer surgery and enlarged prostate management. Dr. Ramani advocates the advantages of robotic surgery-magnified 3D vision, tremor-filtered precision, minimal scarring, lower blood loss and faster recovery-helping patients return to life sooner.
Table of Contents
Recent Blogs
Best Uro-Oncological surgeon
Specialist in India for Robotic Surgery
MCh, DNB, MS, DNB
Dr. Anup Ramani
CONTACT
Uro-Oncologist in India,
Best Robotic Surgeon for Uro Oncology Surgery
1407, One Lodha Place Next to World Towers Senapati Bapat Marg, Worli, Mumbai. 400013.
Dr Anup Ramani @ Copyright 2024 – Website Maintenance, SEO & GEO by Opal Infotech
- Partial penectomy is done in cases where glans and distal penis is involved with carcinoma.
- Partial penectomy is a type of organ-preserving surgery. Preservation of sexual and micturational function depends on the surgical dissection and reconstruction of residual urethra.
- Patients who develop stones in the kidney or ureter, often experience severe pain.
- This condition usually needs a procedure to remove the kidney stones.
- This procedure is called ureteroscopy and is performed very commonly.
- It does not require any cuts and hence it is painless.
- The procedure is performed with an endoscope inserted through the penis under spinal anesthesia.
- The scope is inserted through the penis into the kidney and stones are dissolved with a laser.
- The procedure takes about 40-50 minutes.
- A catheter (urine pipe) is kept after the procedure to drain the bladder. A stent is kept in the kidney at the same time.
- Patient is mobile and walking in the room the same evening.
- Hospital stay is one night and patient is discharged the next day after removal of the catheter.
- Patient has to come back after six weeks to remove the stent in the kidney.
- Patients can resume office a week after surgery and heavy activities like running, weight lifting, a month after the procedure.
- We offer fixed packages for this procedure which can be obtained by calling our helpline +91 9967666060.
- Men with an enlarged prostate, which is a normal ageing changes, often experiencing difficulty passing urine. This condition usually needs a procedure to trim the prostate and relieve the blockage.
- This procedure is called TURP and is performed very commonly.
- It does not require any cuts and hence it is painless.
- The procedure is performed with an endoscope inserted through the penis under spinal anaesthesia.
- The overgrown prostate is dissolved with a laser bloodlessly.
- The procedure takes about 40 minutes.
- A catheter (urine pipe) is kept after the procedure to drain the bladder.
- Patient is mobile and walking in the room the same evening.
- Hospital stay is two nights and patient is discharged with the catheter, which is removed after 4 days.
- Patients can resume office a week after surgery and heavy activities like running, weight lifting, a month after the procedure.
- We offer fixed packages for this procedure which can be obtained by calling our helpline +91 9967666060.
-
Robotic adrenalectomy is a sophisticated, complex surgery and it is very important that an experienced surgeon performs this surgery to avoid major complications.
-
Once the anesthesia is done, and patient positioned, three micro cuts (3mm each) are made in the patient’s abdomen.
-
The arms of the Da Vinci robot are connected to the cuts via ports (tubes).
-
Dr. Ramani then sits in the controlling console to perform the surgery.
-
On an average, a robotic adrenalectomy takes one hour.
-
The surgery is almost completely bloodless and there has never been any need to transfuse blood after surgery.
-
A urine catheter and bag to drain the bladder is inserted during surgery.
-
A tiny drain pipe may be inserted in the surgical side of the abdomen, connected to a bag.
-
Patient is kept nil-by-mouth the day of the surgery, with IV fluids. Sips of water are started the next day and solid food by day three.
-
The drain pipe, if kept, is removed in the room on day 2 after surgery.
-
The catheter is removed on day two after surgery.
-
Total hospital stay for robotic adrenalectomy is 4 nights (including night before surgery).
-
Post discharge, a doctor from the surgical team visits the patient at home/ hotel room once every day.
On the day of discharge, patient is totally self-sufficient. They are able to walk freely without any pain, dress themselves, shower, toilet and they do not need to hire any nurse or help at home. Almost all patients are back to work within 2 weeks of surgery.
Heavy activities like running, weight lifting can be resumed after a month
Follow up after an adrenalectomy is in the form of CT scans, once a year for 5 years.
Local patients usually meet Dr. Ramani after two weeks to discuss report.Outstation patients are counselled on a phone consultation.
- Dr. Ramani is one of the very few surgeons in India who has the expertise to perform a robotic surgery for bladder cancer, which includes removing the urinary bladder and reconstructing a new bladder robotically.
- Robotic radical cystectomy is an extremely sophisticated, complex surgery and it is very important that an experienced surgeon performs this surgery to avoid major complications.
- Once the anaesthesia is done, and patient positioned, six micro cuts (3mm each) are made in the patient’s abdomen.
- The arms of the Da Vinci robot are connected to the cuts via ports (tubes).
- Dr. Ramani then sits in the controlling console to perform the surgery.
- On an average, a robotic radical cystectomy with an ileal conduit takes 3-4 hours.
- The surgery is almost completely bloodless and there has never been any need to transfuse blood after surgery.
- A urine catheter and bag to drain the new bladder is inserted during surgery.
- Two tiny drain pipe in inserted in the surgical side of the abdomen, connected to a bag.
- Patient is kept nil-by-mouth for 4 days after surgery with IV supplementation of patient’s daily requirements of calories, fats, carbohydrates, proteins and electrolytes.
- The drain pipes are removed in the room on day 3-5 after surgery.
- Total hospital stay for radical cystectomy is 8 nights (including night before surgery).
- Post discharge, a doctor from the surgical team visits the patient at home/ hotel room once every day.
- On the day of discharge, patient is totally self-sufficient. They are able to walk freely without any pain, dress themselves, shower, toilet and they do not need to hire any nurse or help at home.
- Almost all patients are back to work within 6 weeks of surgery. Heavy activities like running, weight lifting can be resumed after two months.
Follow up after a radical a cystectomy is in the form of CT scans, once a year for 5 years.
Histopathology report: Local patients usually meet Dr. Ramani after two weeks to discuss report.
Outstation patients are counselled on a phone consult. Depending on the report, patient may or may not need chemotherapy after surgery.
If chemo is needed, patients may choose to get it done with a medical oncologist of their choice or avail the services of one of the four medical oncologists on our team.
- Robotic partial nephrectomy is a sophisticated, complex surgery and it is very important that an experienced surgeon performs this surgery to avoid major complications. Robotic radical (total) nephrectomy is
- relatively easier but still requires significant experience to consistently deliver results.
- Once the anaesthesia is done, and patient positioned, five micro cuts (3mm each) are made in the patient’s abdomen.
- The arms of the Da Vinci robot are connected to the cuts via ports (tubes).
- Dr. Ramani then sits in the controlling console to perform the surgery.
- On an average, a robotic radical nephrectomy takes one hour and a robotic partial nephrectomy takes about an hour and half.
- The surgery is almost completely bloodless and there has never been any need to transfuse blood after surgery.
- A urine catheter and bag to drain the bladder is inserted during surgery.
- A tiny drain pipe in inserted in the surgical side of the abdomen, connected to a bag.
- Patient is kept nil-by-mouth the day of the surgery, with IV fluids. Sips of water are started the next day and solid food by day three.
- The drain pipe is removed in the room on day 3 after surgery. The catheter is removed on day two after surgery.
- Total hospital stay for radical/partial nephrectomy is 4 nights (including night before surgery).
- Post discharge, a doctor from the surgical team visits the patient at home/ hotel room once every day.
- On the day of discharge, patient is totally self- sufficient.
- They are able to walk freely without any pain, dress themselves, shower, toilet and they do not need to hire any nurse or help at home.
- Almost all patients are back to work within 2-3 weeks of surgery.
- Heavy activities like running, weight lifting can be resumed after a month.
- Follow up after a radical/partial Nephrectomy is in the form of CT scans, once a year for 5 years.
- Local patients usually meet Dr. Ramani after two weeks to discuss report.
- Outstation patients are counselled on a phone consultation.