Dr Anup Ramani @ Copyright 2024
By Dr. Anup Ramani
Objective
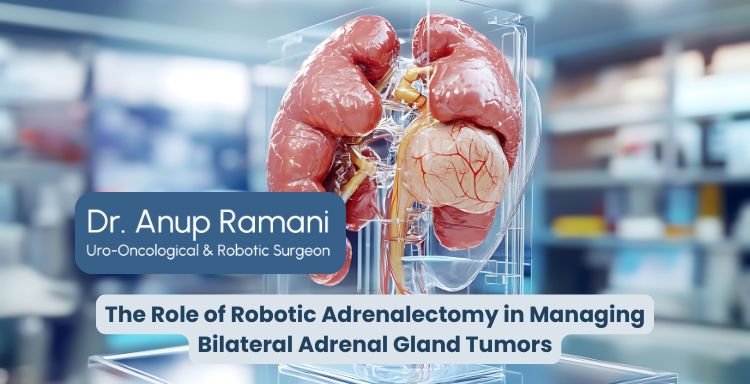
Bilateral adrenal gland tumors pose a unique challenge due to the complexity of operating on both adrenal glands, especially when critical blood vessels and surrounding organs are involved. Robotic adrenalectomy offers a precise, minimal invasive solution that enhances surgical safety, preserves hormonal function and ensures better outcomes. This article explores how robotic adrenalectomy surgery has transformed adrenal gland treatment, particularly for patients with bilateral tumors.
Understanding Bilateral Adrenal Gland Tumors and Their Surgical Challenges
Bilateral adrenal gland tumors occur when growths are present in both adrenal glands. Though relatively rare, these tumors can lead to serious health issues including hormone imbalances, high blood pressure, Cushing’s syndrome or pheochromocytoma. Because the adrenal glands control essential hormone production – cortisol, aldosterone and adrenaline – tumors in both glands require extremely careful handling during surgery.
Surgical intervention becomes even more complex in bilateral cases due to the need to preserve enough healthy adrenal tissue to maintain hormonal balance. Completely removing both glands can result in adrenal insufficiency, requiring lifelong hormone replacement therapy. Furthermore, the adrenal glands lie deep within the abdomen, close to critical structures like the inferior vena cava, kidneys, pancreas and spleen. Any surgical misstep in this area could lead to severe complications such as internal bleeding or organ damage.
Conventional open adrenal gland surgery for bilateral tumors involves large incisions, extended hospital stays and higher risks of complications. Even laparoscopic approaches, while less invasive, lack the level of precision needed for bilateral adrenal tumor resection without compromising surrounding tissues. This is where robotic adrenalectomy steps in as a superior alternative.
Read Our Article :
Life After Adrenalectomy: Hormone Management and Long-Term Care
Why Robotic Adrenalectomy Is Preferred Over Traditional Surgery for Bilateral Tumors
Robotic adrenalectomy has emerged as the preferred technique for managing complex adrenal conditions, particularly when both adrenal glands are involved. Traditional surgery, while effective in select cases, does not offer the same degree of control, visualization or precision that robotic systems provide. For bilateral adrenal tumors, these advantages become critical.
Robotic adrenalectomy surgery allows an adrenal gland surgeon to operate with 3D high-definition vision and greater magnification, which is essential for identifying the delicate structures surrounding the adrenal glands. The robotic instruments used in the procedure offer a range of motion far superior to the human hand, enabling more refined dissection of tumors from sensitive tissues.
With robotic assistance, it’s also possible to perform staged or simultaneous adrenalectomies, depending on the patient’s condition and tumor characteristics. This flexibility is particularly beneficial in minimizing stress on the body and reducing the likelihood of long-term hormonal issues.
Robotic adrenalectomy surgeons report lower conversion rates to open surgery, shorter operative times and fewer intraoperative complications in bilateral adrenal surgeries. In experienced hands, robotic adrenalectomy treatment offers a safe, effective path to managing these high-risk tumors with less pain, faster recovery and better long-term outcomes.
What Our Patients Are Saying
Precision Handling of Critical Blood Vessels During Robotic Adrenal Surgery
One of the most significant challenges in adrenal gland surgery – especially bilateral cases – is managing the dense vascular structures that surround the adrenal glands. These include the adrenal veins, renal arteries and the inferior vena cava. Accidental injury to these vessels can result in life-threatening bleeding or organ dysfunction.
Robotic adrenalectomy technology provides unmatched precision in navigating these critical areas. The 3D imaging and articulated robotic arms enable surgeons to make extremely fine movements, which are crucial when working within millimetres of major vessels. The enhanced dexterity of the instruments allows for delicate dissection and cauterization without causing trauma to surrounding blood vessels or tissues.
In addition to greater precision, robotic adrenalectomy also offers better control of bleeding. Surgeons can carefully seal small vessels as they proceed, reducing blood loss and maintaining a clear surgical field. This is particularly important in bilateral adrenal surgeries, where maintaining visibility and vessel integrity on both sides of the body is essential.
With robotic adrenalectomy treatment, the risk of haemorrhage, vascular injury or unintended damage to adjacent organs is significantly lowered. This creates a safer surgical environment for patients with complex adrenal pathologies and contributes to more predictable, controlled surgical outcomes.
Organ-Preserving Techniques: Protecting Healthy Adrenal Tissue with Robotics
In bilateral adrenal gland tumor cases, one of the key goals is to preserve as much healthy adrenal tissue as possible to maintain hormone production and avoid lifelong dependency on steroid medications. Robotic adrenalectomy makes organ-preserving techniques more feasible through superior visualization and fine-tuned surgical control.
Unlike open surgery, where it’s difficult to isolate and remove only the tumor without harming adjacent tissue, robotic systems allow adrenal gland surgeons to perform partial adrenalectomy. This involves removing just the tumor or hyperactive portion of the gland while sparing the remaining healthy tissue. Such precision is especially useful in patients with hereditary conditions.
Read Our Article :
Understanding the Safety and Success Rates of Robotic Adrenal Gland Surgery
Adrenal Gland Surgery gives the surgeon a distinct advantage in this regard. By using advanced instruments that mimic human wrist movement but at a much finer scale, surgeons can delicately separate tumor tissue from functioning adrenal cortex. Additionally, intraoperative imaging and hormone level monitoring can guide the extent of tissue removal.
Organ-preserving robotic adrenalectomy treatment not only reduces the chances of postoperative adrenal insufficiency but also allows patients to retain a more normal quality of life. This technique represents a major step forward in adrenal gland surgery, especially for bilateral cases where full gland removal carries significant long-term risks.
Reduced Risk of Complications in Bilateral Adrenal Gland Surgeries with Robotic Technology
Managing tumors in both adrenal glands raises the stakes for surgical complications, including bleeding, infection organ injury and postoperative hormonal imbalance. Robotic adrenalectomy significantly lowers these risks, making it a safer option for complex bilateral surgeries.
One of the primary reasons for this improved safety profile is the reduced physical trauma associated with robotic adrenalectomy surgery. Smaller incisions, minimal tissue handling and precise movements result in less inflammation and reduced risk of postoperative infection. The surgical site remains cleaner and recovery is typically quicker.
Furthermore, adrenal gland surgeons have greater control over critical decisions during surgery, such as when to stop dissection, how much tissue to preserve and how to handle unexpected anatomical variations. These decisions, when made with real-time high-resolution visuals and robotic assistance, are far more accurate than in conventional surgery.
In bilateral surgeries, the potential for adrenal crisis due to loss of hormonal production is also a concern. Robotic systems enable better preservation of gland function and allow for careful resection planning, which minimizes the likelihood of this complication.
The result is fewer hospital readmissions, reduced need for blood transfusions and lower dependency on post-operative hormone therapy – key indicators of successful adrenal gland treatment.
Post-Surgery Outcomes: Hormonal Stability and Recovery After Robotic Bilateral Adrenalectomy
Postoperative recovery and long-term hormonal stability are top priorities in any adrenal gland treatment plan, especially when both glands are involved. Robotic adrenalectomy delivers excellent outcomes on both fronts, offering patients a quicker return to health and more stable hormone levels after surgery.
Because the robotic approach is less invasive, patients typically experience minimal postoperative pain and are discharged within 24 to 48 hours. Recovery time is significantly shortened compared to open surgery and most patients return to normal activities within 1 to 2 weeks.
Hormonal management is also more predictable after robotic adrenalectomy. Whether the procedure involves full or partial gland removal, surgeons can plan resection with high precision to preserve as much adrenal function as possible. In cases where total bilateral adrenalectomy is necessary, patients are better prepared for hormone replacement due to the controlled, step-by-step nature of robotic surgery.
Studies have shown that patients who undergo robotic adrenalectomy surgery for bilateral tumors have fewer complications and more consistent hormonal stabilization post-surgery. Many leading centers offering adrenal gland treatment in India are now adopting robotic techniques as the standard for bilateral adrenal pathologies due to these favorable outcomes.
Overall, adrenal gland treatment represents a significant leap forward in endocrine surgery, especially for complex bilateral adrenal tumor cases where precision, safety and recovery are paramount.
FAQs: About Robotic Adrenectomy
What is robotic adrenalectomy?
It is a minimal invasive surgery that uses robotic technology to remove adrenal gland tumors with high precision and safety.
Why is robotic adrenalectomy preferred for bilateral adrenal tumors?
Because it offers better control, lower risk of complications and improved preservation of healthy adrenal tissue.
Can robotic adrenalectomy help avoid lifelong hormone therapy?
Yes, especially in partial adrenalectomy cases where enough adrenal tissue is preserved to maintain hormonal balance.
What are the recovery benefits of robotic adrenalectomy surgery?
Patients experience less pain, shorter hospital stays and faster return to daily life compared to traditional surgery.
About Author

Uro-Oncological & Robotic Surgeon
Dr. Anup Ramani is a robotic uro-oncological surgeon and an internationally recognized expert in robotic surgery for prostate, kidney and urinary bladder cancers. With more than two decades of robotic experience and 2,000+ robotic procedures, he brings unmatched precision and outcomes to complex uro-oncology cases. He is widely published in his field and is known for a personal, transparent approach-often spending over an hour in initial consultations to educate patients on its disease, surgery and recovery. His expertise spans prostate cancer treatment, kidney and bladder cancer surgery, adrenal gland surgery, kidney stone treatment, penile cancer surgery and enlarged prostate management. Dr. Ramani advocates the advantages of robotic surgery-magnified 3D vision, tremor-filtered precision, minimal scarring, lower blood loss and faster recovery-helping patients return to life sooner.
Table of Contents
Recent Blogs
Best Uro-Oncological surgeon
Specialist in India for Robotic Surgery
MCh, DNB, MS, DNB
Dr. Anup Ramani
CONTACT
Uro-Oncologist in India,
Best Robotic Surgeon for Uro Oncology Surgery
1407, One Lodha Place Next to World Towers Senapati Bapat Marg, Worli, Mumbai. 400013.
Dr Anup Ramani @ Copyright 2024 – Website Maintenance, SEO & GEO by Opal Infotech
- Partial penectomy is done in cases where glans and distal penis is involved with carcinoma.
- Partial penectomy is a type of organ-preserving surgery. Preservation of sexual and micturational function depends on the surgical dissection and reconstruction of residual urethra.
- Patients who develop stones in the kidney or ureter, often experience severe pain.
- This condition usually needs a procedure to remove the kidney stones.
- This procedure is called ureteroscopy and is performed very commonly.
- It does not require any cuts and hence it is painless.
- The procedure is performed with an endoscope inserted through the penis under spinal anesthesia.
- The scope is inserted through the penis into the kidney and stones are dissolved with a laser.
- The procedure takes about 40-50 minutes.
- A catheter (urine pipe) is kept after the procedure to drain the bladder. A stent is kept in the kidney at the same time.
- Patient is mobile and walking in the room the same evening.
- Hospital stay is one night and patient is discharged the next day after removal of the catheter.
- Patient has to come back after six weeks to remove the stent in the kidney.
- Patients can resume office a week after surgery and heavy activities like running, weight lifting, a month after the procedure.
- We offer fixed packages for this procedure which can be obtained by calling our helpline +91 9967666060.
- Men with an enlarged prostate, which is a normal ageing changes, often experiencing difficulty passing urine. This condition usually needs a procedure to trim the prostate and relieve the blockage.
- This procedure is called TURP and is performed very commonly.
- It does not require any cuts and hence it is painless.
- The procedure is performed with an endoscope inserted through the penis under spinal anaesthesia.
- The overgrown prostate is dissolved with a laser bloodlessly.
- The procedure takes about 40 minutes.
- A catheter (urine pipe) is kept after the procedure to drain the bladder.
- Patient is mobile and walking in the room the same evening.
- Hospital stay is two nights and patient is discharged with the catheter, which is removed after 4 days.
- Patients can resume office a week after surgery and heavy activities like running, weight lifting, a month after the procedure.
- We offer fixed packages for this procedure which can be obtained by calling our helpline +91 9967666060.
-
Robotic adrenalectomy is a sophisticated, complex surgery and it is very important that an experienced surgeon performs this surgery to avoid major complications.
-
Once the anesthesia is done, and patient positioned, three micro cuts (3mm each) are made in the patient’s abdomen.
-
The arms of the Da Vinci robot are connected to the cuts via ports (tubes).
-
Dr. Ramani then sits in the controlling console to perform the surgery.
-
On an average, a robotic adrenalectomy takes one hour.
-
The surgery is almost completely bloodless and there has never been any need to transfuse blood after surgery.
-
A urine catheter and bag to drain the bladder is inserted during surgery.
-
A tiny drain pipe may be inserted in the surgical side of the abdomen, connected to a bag.
-
Patient is kept nil-by-mouth the day of the surgery, with IV fluids. Sips of water are started the next day and solid food by day three.
-
The drain pipe, if kept, is removed in the room on day 2 after surgery.
-
The catheter is removed on day two after surgery.
-
Total hospital stay for robotic adrenalectomy is 4 nights (including night before surgery).
-
Post discharge, a doctor from the surgical team visits the patient at home/ hotel room once every day.
On the day of discharge, patient is totally self-sufficient. They are able to walk freely without any pain, dress themselves, shower, toilet and they do not need to hire any nurse or help at home. Almost all patients are back to work within 2 weeks of surgery.
Heavy activities like running, weight lifting can be resumed after a month
Follow up after an adrenalectomy is in the form of CT scans, once a year for 5 years.
Local patients usually meet Dr. Ramani after two weeks to discuss report.Outstation patients are counselled on a phone consultation.
- Dr. Ramani is one of the very few surgeons in India who has the expertise to perform a robotic surgery for bladder cancer, which includes removing the urinary bladder and reconstructing a new bladder robotically.
- Robotic radical cystectomy is an extremely sophisticated, complex surgery and it is very important that an experienced surgeon performs this surgery to avoid major complications.
- Once the anaesthesia is done, and patient positioned, six micro cuts (3mm each) are made in the patient’s abdomen.
- The arms of the Da Vinci robot are connected to the cuts via ports (tubes).
- Dr. Ramani then sits in the controlling console to perform the surgery.
- On an average, a robotic radical cystectomy with an ileal conduit takes 3-4 hours.
- The surgery is almost completely bloodless and there has never been any need to transfuse blood after surgery.
- A urine catheter and bag to drain the new bladder is inserted during surgery.
- Two tiny drain pipe in inserted in the surgical side of the abdomen, connected to a bag.
- Patient is kept nil-by-mouth for 4 days after surgery with IV supplementation of patient’s daily requirements of calories, fats, carbohydrates, proteins and electrolytes.
- The drain pipes are removed in the room on day 3-5 after surgery.
- Total hospital stay for radical cystectomy is 8 nights (including night before surgery).
- Post discharge, a doctor from the surgical team visits the patient at home/ hotel room once every day.
- On the day of discharge, patient is totally self-sufficient. They are able to walk freely without any pain, dress themselves, shower, toilet and they do not need to hire any nurse or help at home.
- Almost all patients are back to work within 6 weeks of surgery. Heavy activities like running, weight lifting can be resumed after two months.
Follow up after a radical a cystectomy is in the form of CT scans, once a year for 5 years.
Histopathology report: Local patients usually meet Dr. Ramani after two weeks to discuss report.
Outstation patients are counselled on a phone consult. Depending on the report, patient may or may not need chemotherapy after surgery.
If chemo is needed, patients may choose to get it done with a medical oncologist of their choice or avail the services of one of the four medical oncologists on our team.
- Robotic partial nephrectomy is a sophisticated, complex surgery and it is very important that an experienced surgeon performs this surgery to avoid major complications. Robotic radical (total) nephrectomy is
- relatively easier but still requires significant experience to consistently deliver results.
- Once the anaesthesia is done, and patient positioned, five micro cuts (3mm each) are made in the patient’s abdomen.
- The arms of the Da Vinci robot are connected to the cuts via ports (tubes).
- Dr. Ramani then sits in the controlling console to perform the surgery.
- On an average, a robotic radical nephrectomy takes one hour and a robotic partial nephrectomy takes about an hour and half.
- The surgery is almost completely bloodless and there has never been any need to transfuse blood after surgery.
- A urine catheter and bag to drain the bladder is inserted during surgery.
- A tiny drain pipe in inserted in the surgical side of the abdomen, connected to a bag.
- Patient is kept nil-by-mouth the day of the surgery, with IV fluids. Sips of water are started the next day and solid food by day three.
- The drain pipe is removed in the room on day 3 after surgery. The catheter is removed on day two after surgery.
- Total hospital stay for radical/partial nephrectomy is 4 nights (including night before surgery).
- Post discharge, a doctor from the surgical team visits the patient at home/ hotel room once every day.
- On the day of discharge, patient is totally self- sufficient.
- They are able to walk freely without any pain, dress themselves, shower, toilet and they do not need to hire any nurse or help at home.
- Almost all patients are back to work within 2-3 weeks of surgery.
- Heavy activities like running, weight lifting can be resumed after a month.
- Follow up after a radical/partial Nephrectomy is in the form of CT scans, once a year for 5 years.
- Local patients usually meet Dr. Ramani after two weeks to discuss report.
- Outstation patients are counselled on a phone consultation.